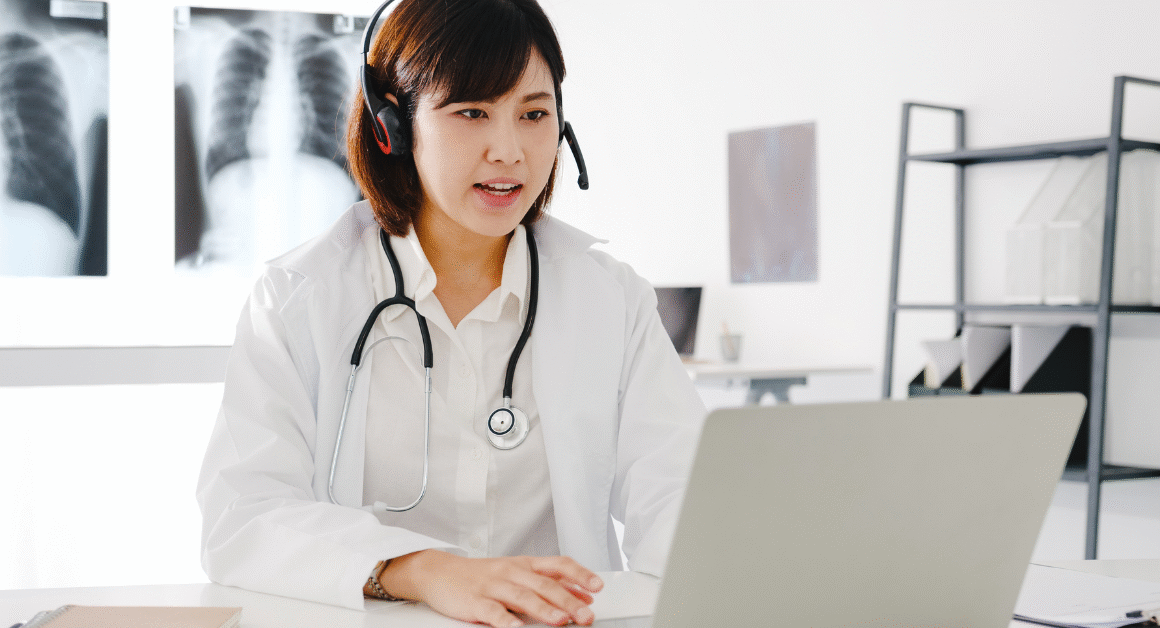
The Centers for Medicare & Medicaid Services (CMS) is set to broaden its Medicare prior authorization requirements to include ambulatory surgical centers (ASCs) in ten states beginning December 2025. This new policy aims to improve patient safety and reduce unnecessary procedures by carefully reviewing certain services before they are performed. For many patients and healthcare providers, understanding these changes will be crucial in navigating the Medicare system smoothly.
Ambulatory surgical centers provide outpatient surgical care, which means patients do not have to stay overnight. With the new expansion of prior authorization, more treatments and procedures will require approval from Medicare beforehand. This step is part of a broader national effort to control healthcare costs while ensuring the quality of care across different medical settings.
What is Medicare Prior Authorization?
Medicare prior authorization is a process where healthcare providers must get approval from Medicare before performing specific medical procedures, tests, or services. This helps Medicare verify that the services are necessary and meet certain guidelines before paying for them. The goal is to avoid unnecessary treatments and save costs without compromising patient health.
Originally, prior authorization was mainly required for inpatient hospital stays and some home health services, but recent updates have expanded its scope. The expansion to ambulatory surgical centers means more outpatient procedures will now fall under prior authorization rules.
Which States Are Affected?
Starting December 2025, ten states will see this expansion for ASCs under Medicare prior authorization. The states include California, Florida, Texas, New York, Pennsylvania, Ohio, Georgia, North Carolina, Michigan, and Illinois. These states were selected due to their large populations and high volume of outpatient surgical services.
Healthcare providers and patients in these states should prepare for additional paperwork and wait times before many ASC procedures. Knowing this in advance can help patients plan their surgeries to avoid delays and ensure smooth communication with their doctors.
How Will This Impact Patients and Providers?
For patients, the biggest change is that some surgeries or procedures performed in ambulatory surgical centers will need Medicare’s approval ahead of time. This means it is important to check with your healthcare provider if prior authorization is required for your specific procedure to avoid unexpected denials or delays.
For healthcare providers, especially those operating in ASCs, the new policy adds administrative tasks and requires familiarity with the updated Medicare prior authorization system. Providers must submit necessary information timely to avoid delays in patient care. However, this can also lead to fewer unnecessary procedures, improving patient safety and reducing costs.
Why Did Medicare Expand Prior Authorization to ASCs?
The move to expand prior authorization to ambulatory surgical centers is part of Medicare’s ongoing effort to improve care quality and control healthcare spending. According to CMS, prior authorization helps prevent improper payments and supports better healthcare decisions by ensuring only necessary procedures are approved.
Studies have also shown that prior authorization programs can reduce the use of low-value care without negatively impacting patients’ health outcomes. By including ASCs, Medicare hopes to extend these benefits to outpatient surgical settings, which are growing in use nationwide.
What Should Patients Do to Prepare?
Patients with upcoming ASC procedures in the affected states should speak with their doctors well in advance to understand if prior authorization is needed. It’s important to have clear communication between you, your healthcare provider, and Medicare to avoid surprises.
Keep track of any documents or approvals related to your procedure, and don’t hesitate to ask your provider about the prior authorization process. Being proactive can help ensure your surgery or treatment happens on time without unnecessary delays.
Where Can You Find More Information?
For detailed and official information, it’s best to visit the Centers for Medicare & Medicaid Services website, which offers comprehensive guides and updates on prior authorization. The CMS Medicare Prior Authorization webpage is a great resource for both patients and providers.
Additionally, the Kaiser Family Foundation provides accessible summaries explaining the expansion and its implications, which can be helpful for general understanding.
References: CMS Medicare Prior Authorization for ASCs, Kaiser Family Foundation Medicare Prior Authorization