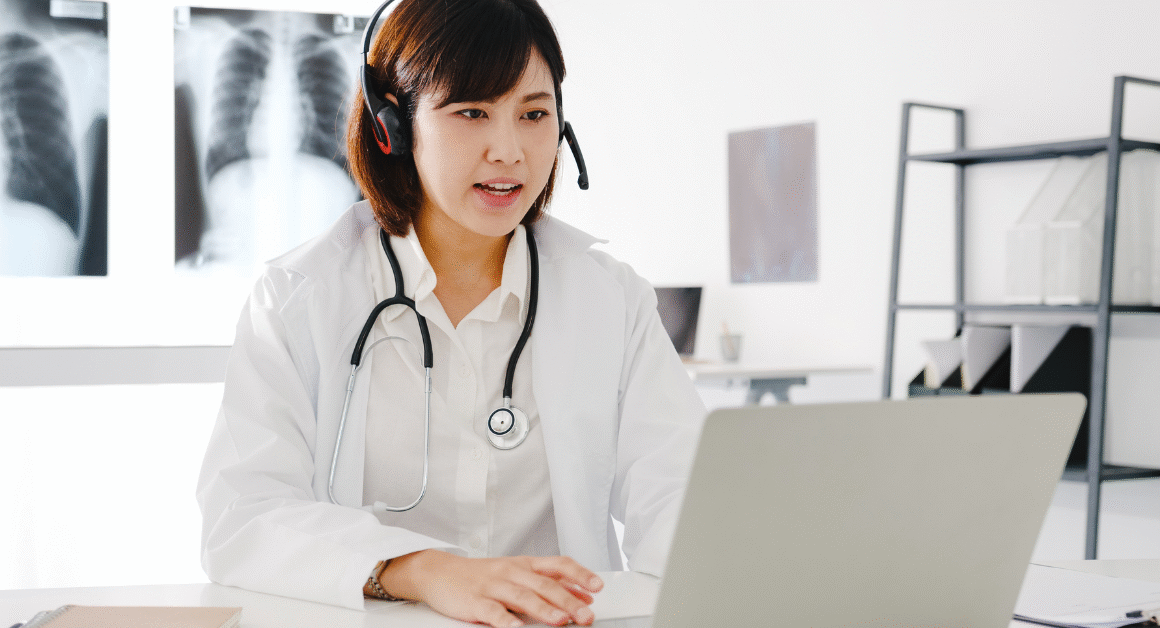
The 2025 budget reconciliation law brings significant changes for Medicaid recipients across the United States. Among these are new work requirements and verification mandates designed to reshape how Medicaid eligibility is monitored. These updates will impact millions of people, making it crucial to understand what the changes mean and how they might affect access to healthcare coverage.
The Kaiser Family Foundation (KFF), a trusted source for health policy information, is closely tracking these new mandates. Their insights help explain the complex details of the law, ensuring that both policymakers and the public stay informed about Medicaid’s evolving landscape. This article breaks down the key points of the 2025 Medicaid work and verification changes and explores their potential effects.
Understanding Medicaid Work Requirements
Medicaid work requirements are rules that ask recipients to engage in certain activities like paid employment, job training, or community service to remain eligible for benefits. These requirements aim to encourage beneficiaries to enter or stay in the workforce. The 2025 budget reconciliation law reintroduces and expands these work mandates for Medicaid recipients in many states.
KFF explains that while work requirements have been proposed before, they often faced legal challenges and debate about their effectiveness. The new law attempts to implement these rules more consistently, with strict verification processes to ensure compliance. This means many Medicaid recipients will need to prove they meet these work or activity criteria regularly.
Verification Mandates and How They Work
Verification mandates are the system’s way to check that Medicaid recipients are meeting the new work requirements. The 2025 law outlines specific procedures for states to follow. This includes gathering documentation such as pay stubs, employer reports, or proof of enrollment in training programs. The government’s goal is to reduce fraud and ensure Medicaid funds assist those actively working or participating in approved activities.
However, these verification processes could also create challenges for Medicaid recipients. For example, those juggling multiple jobs or informal work arrangements might struggle to provide consistent proof. KFF notes that without clear guidance and support, some individuals could lose coverage despite meeting the spirit of the requirements.
Impact on Medicaid Beneficiaries and States
The new mandates affect not only individuals but also state governments administering Medicaid programs. States must develop or improve systems to track work activities, gather verification documents, and enforce compliance. This may require significant administrative changes and increased funding.
For Medicaid beneficiaries, these requirements could mean extra paperwork, the need to report employment status regularly, and the risk of losing coverage if verification processes are not completed successfully. Many advocates worry that the new work and verification rules might disproportionately impact vulnerable populations, including people with disabilities and those experiencing unstable employment.
What Experts Are Saying
Health policy experts at the Kaiser Family Foundation and other organizations highlight mixed views on the effectiveness of work requirements. Some suggest that while the goal of encouraging employment is positive, the realities of poverty and job instability make strict mandates problematic. The Urban Institute also points out that work requirements have often led to coverage losses without significant increases in employment rates.
These concerns emphasize the need for states and federal officials to provide clear guidance, support services, and exceptions where necessary. The balance between encouraging work and maintaining access to healthcare is delicate, requiring careful policy design and ongoing monitoring.
How to Stay Informed and Engage
If you or someone you know is on Medicaid, it’s important to stay updated on these changes. Visiting trustworthy sources like the Kaiser Family Foundation’s website can provide timely news and detailed explanations of how the 2025 mandates may apply in your state. Additionally, local health departments and Medicaid offices will offer guidance on how to comply with new work and verification rules.
Advocacy groups and community organizations often provide help in navigating the verification process and understanding exemptions. Engaging with these resources can make a difference in successfully maintaining Medicaid coverage under the new mandates.
Conclusion
The 2025 budget reconciliation law’s Medicaid work and verification mandates represent a major shift in healthcare policy. While the intentions focus on promoting employment and accountability, the practical challenges for recipients and states are significant. Ongoing tracking by organizations like the Kaiser Family Foundation helps clarify these complex changes. Staying informed and seeking help when needed will be key to navigating this new Medicaid environment.