The healthcare industry is preparing for significant changes as the Centers for Medicare & Medicaid Services (CMS) introduces stricter quality metrics for health insurers. These updates will influence bonus payments starting in the 2026 plan year. Health insurers must now focus more than ever on improving patient care quality to secure incentive payments and maintain competitive advantages.
With these enhanced requirements, insurers will need to pay close attention to new performance standards set by CMS. Understanding the impact of these changes is essential for providers, payers, and patients alike. This article dives into what the new CMS quality metrics mean for health insurers and how the industry is gearing up for these challenges.
What Are CMS Quality Metrics?
CMS quality metrics are a set of performance measures used to evaluate health plans’ effectiveness in delivering healthcare services. These metrics focus on different areas such as patient experience, preventive care, chronic condition management, and health outcomes. Health insurers receive bonus payments based on how well they perform against these metrics, encouraging better care for beneficiaries.
According to the Centers for Medicare & Medicaid Services (CMS), these quality metrics aim to promote value-based care instead of volume-based care, meaning providers get rewarded for quality results rather than the quantity of services rendered.
Stricter Metrics Ahead of 2026 Bonus Payments
Starting with the 2026 plan year, CMS plans to implement more rigorous quality standards for health insurers. These tougher benchmarks will raise the bar on how insurers manage patient outcomes, improve preventive health services, and reduce health disparities among populations.
The new metrics will demand higher scores in areas such as controlling blood pressure, managing diabetes, and addressing mental health issues. CMS also plans to place greater emphasis on social determinants of health, encouraging insurers to address factors like housing, nutrition, and access to care, which directly affect patient well-being.
Impact on Health Insurers and Beneficiaries
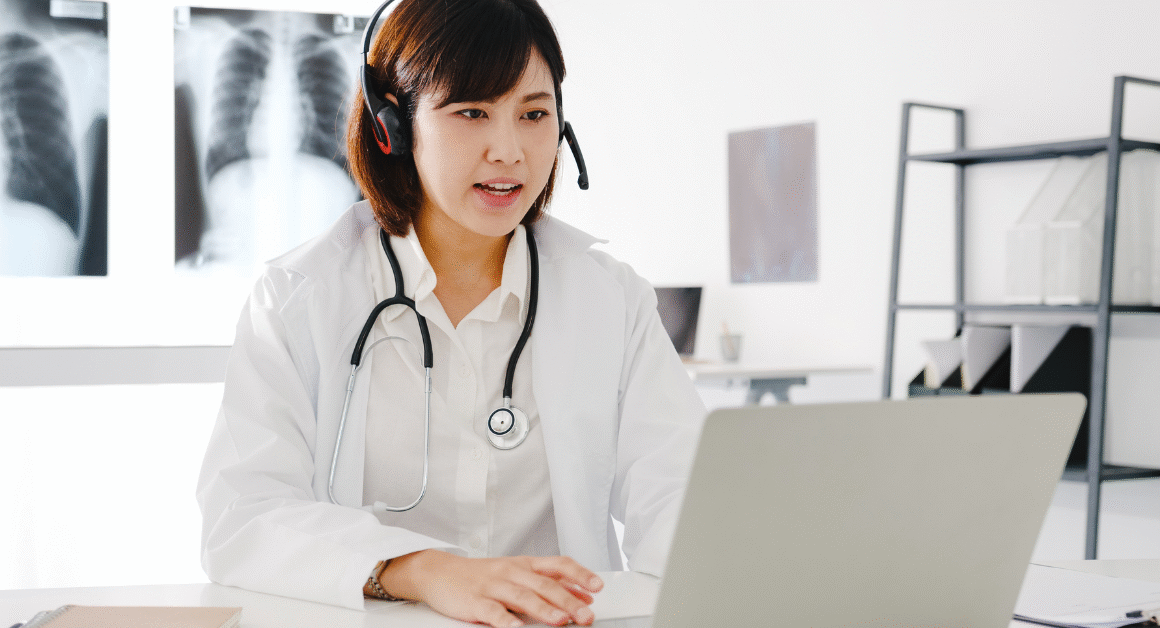
These upcoming changes mean health insurers need to invest in better data management, patient engagement strategies, and innovative care models. As Health Affairs reports, insurers striving to meet stricter CMS standards are incorporating more technology-driven solutions like telemedicine, predictive analytics, and personalized care plans to improve quality scores.
For beneficiaries, this shift promises enhanced access to preventive and coordinated care, leading to better health outcomes and fewer unnecessary hospital visits. However, it may also result in insurers focusing resources on high-risk patients to improve overall performance on quality metrics.
Challenges and Opportunities
While stricter CMS quality metrics can be challenging, they also present opportunities for health insurers. By focusing on quality of care, insurers can differentiate themselves in a competitive market and build stronger patient trust. Additionally, improving health outcomes can lower long-term healthcare costs for both insurers and patients.
At the same time, insurers must overcome obstacles such as integrating complex data systems, addressing health equity, and managing cost increases linked to advanced care models. As Kaiser Family Foundation highlights, collaboration between providers, payers, and community organizations will be key to meeting these new standards effectively.
Preparing for 2026 and Beyond
The best approach for health insurers is to start now by enhancing quality improvement programs, investing in workforce training, and embracing patient-centered care initiatives. Keeping up with CMS updates and leveraging data analytics can help insurers stay ahead of the curve.
Continued efforts to reduce health disparities and improve social determinants will also be critical to successfully meeting the stricter metrics coming in 2026. By focusing on these areas, health insurers can position themselves to earn bonus payments, improve patient satisfaction, and contribute to a healthier population.
Conclusion
The upcoming stricter CMS quality metrics signal an important shift in how health insurers deliver care and measure success. While these changes present challenges, they also offer promising opportunities for improving healthcare quality and patient outcomes. Health insurers who act early to adapt their strategies will be best prepared to thrive in the evolving healthcare landscape ahead.